As a carry-on from my last blog ‘Back Pain – Is it coming from my SI joint?’ let’s look at back pain that is potentially arising from one of the discs between the vertebrae in the low back. When we consider that 70% of our weight-bearing compressive load is taken through the vertebral bodies and discs it is not surprising that pre-test probability shows that 40% of low back pain is attributed to disc lesions. Many people with disc problems come to yoga practice to rebuild stability and strength and to heal and protect themselves from further injury. Sadly, students sometimes incur disc disruptions from over-zealous practice or poorly executed adjustments. The topic of disc anatomy, function and degeneration is extensive and intriguing! It suffices to say that our intervertebral discs are like a hydraulic cushion with an ingenious design – they take large tensile loads, can bend around and when healthy, bounce back! For the sake of brevity this blog focuses on you being able to identify if back pain is coming from a disc that you can then exercise the care needed for an uninterrupted, complete recovery.
CAUSES & RISKS
Interestingly, a 2010 study in the Spine Journal on ‘Inciting events associated with lumbar disc herniation’ found that approximately 60% of people identified no specific event preceding their disc herniation symptoms; 30% reported that their symptoms began after their usually well-tolerated daily routines and only 8% noted symptoms after heavy lifting or specific trauma. A more recent study shows that genetic factors are critical contributors to the onset and progression of disc degeneration. These genetic factors create a susceptibility to the stresses of normal wear and tear and poor postural habits. They cause metabolic changes within the disc which cause it to prematurely and rapidly break down. Combined with aging, cumulative injury (minor or macro), and/or spinal deformity a change in nutrient supply leads to an inability of the nuclear matrix to maintain its hydration. Without the inner cushion of the nucleus the load shifts eccentrically to the annulus (outer fibrocartilage layers of the disc) predisposing it to tears and degeneration.
From an activity point of view one of the main contributors to disc degeneration is having the low back in a static flexed position. This position approximately doubles the normal load on the discs. This is exactly what happens when we sit without lumbar support and/or without the activity of our trunk muscles. In yoga most disc injuries seem to happen in postures where the low back is strongly rounded without sufficient core support, e.g.: Kurmasana and leg-behind-head postures. The most extreme of stresses is in postures like Dwi Pada Śirsasana where one must additionally support the weight of the legs on an already strongly flexed lumbar spine. For this reason, it is imperative to have good trunk strength before attempting these demanding postures.
Twisting the spine does stress the elastin links between the concentric layers of fibres in the annulus of the disc. Ensure that you elongate your spine before performing twisting postures. This unloads the discs by activating the support of the deep stabilizing muscles.
TYPES of DISC DISRUPTIONS
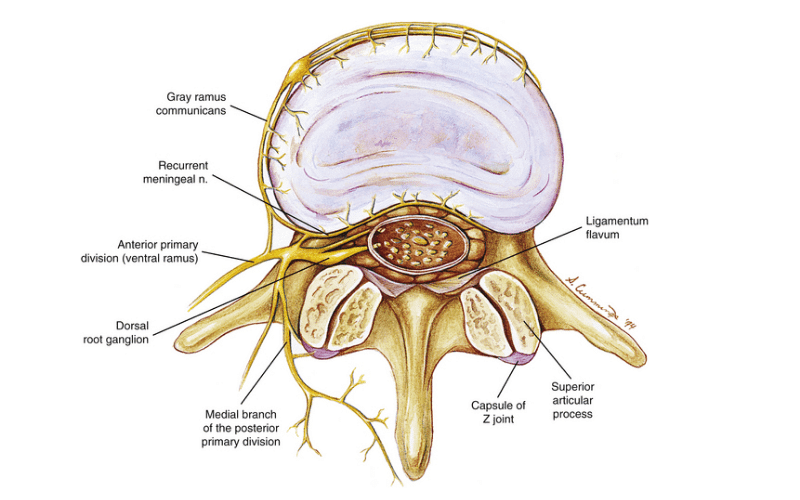
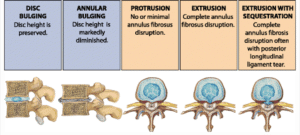
To protect it from harm, the outer 1/3 of the disc (see title picture), where it takes the greatest load, is innervated with sensory nerves which is why structural disc problems are painful and debilitating. Along the path of disc displacements there is a progression of severity with a usually equal progression of pain, dysfunction and recovery time. (See image below). Some amount of disc degeneration is normal from the wear and tear that comes with aging and is often asymptomatic. In fact, our discs are one of the first connective tissues in our body to show signs of degeneration. You can see these first signs in 20% of teenagers!
The first significant sign of disc disruption is termed disc bulging. A disc bulge is when more than 50% of the disc circumference lies beyond the diameter of the vertebral body. Beyond a disc bulge a disruption of the inner gelatinous nucleus of the disc is called a prolapse. A prolapse is defined by the nucleus of the disc still being contained within the outer fibrocartilage layers of the annulus of the disc. When the nucleus extends beyond this fibrous boundary it is called an extrusion. The most severe displacement is when the disc material transverses into the space of the spinal canal. It is then termed an extrusion with sequestration. Our immune response to these “leaky discs” can itself cause a biochemical insult to the nerves and cause pain, even without any contact!
PATTERN OF ONSET & SYMPTOMS
Disc disruptions can have very different patterns of onset of pain and/or disability. Much of this depends on how the disc tears. A tear or fissure can happen between the concentric ring layers of the outer disc where it is highly innervated. In this case there is usually sudden severe pain with an immediate inability to move. It can be accompanied by a click or pop as the elastin glue between the layers gives way. There is often a sudden “locking” that happens when in a position of minimal flexion with slight rotation. When the tear is a split from the centre of the nucleus that radiates out into the periphery of the annulus there can be mild pain or a strange sensation in the low back and gradually over several hours or days one is unable to move as the tear deepens into the sensitive outer 1/3 of the disc.
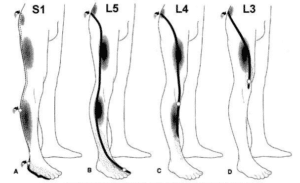
The most relevant categorisation of disc lesions is those that press on the root of a nerve and those that do not. Compression of the thecal sac which contains the spinal cord is also possible if the disc protrusion is towards the back of the vertebra and can cause severe pain as it is highly innervated to protect the spinal cord. Obviously, a disc disruption that does not press on any part of the nervous system is less serious and less painful than one that compresses nerve tissue. Any of the above disruptions of the disc could press on a spinal nerve where it exits between adjoining vertebrae. Compression on a nerve will cause radiating nerve pain down the leg. This symptom of sharp, radiating leg pain is generally named sciatic. However, the body itself gives us a map that helps to determine exactly which nerve is being compromised. This map (dermatomes) express pain along the path of sensory distribution from the nerve at one particular level (see image). We have a little rhyme to help remember these: “S1 on the bun, L5 down the side, L4 on the thigh, L3 to the knee”. Other neurological tests for spinal reflexes, sensory impairment and muscle strength can help to predict the exact level of nerve impingement.
One of the biggest clues that back pain comes from an intervertebral disc is when the pain is experienced centrally along the spine, rather than off to one side, and without superficial tenderness. Most discs behave in the same way in that there is a history of recurrent stiffness and/or prolonged flexion loading. For most the pain is worse when sitting and better when standing and/or walking. Flexion of the spine aggravates it, while extension gives relief. The pain often centralises towards the spine and away from the leg with certain positions or movements. When the disruption is on one side the body will lean away from the painful side in an antalgic stance. Increasing pressure in the dural sac that surrounds the spinal cord by sneezing, coughing or bearing down will aggravate the pain as will the Slump Test. As the disc can protrude and press on a nerve root or the spinal cord the Slump Test is a simple, common diagnostic tool. It aims to stretch the spinal cord. As the nervous system is one continuous tissue from the brain to every nerve end, any compression along its path will be felt when you slump and stretch the entire system.
The Slump Test
Sitting the spine and neck are rounded into a slumped position with the knee extended and the ankle in dorsiflexion. To differentiate this from myofascial tension and pain you can lift your head. If the pain eases it is less likely to be coming from nerve root compression.
THERAPY
The muscles most affected by disc disruptions are the deep (and meaningful J) stabilising muscles of the low back. This group includes the multifidi muscles which are a study unto themselves and their health has been shown to be inversely proportionate to low back pain. In simple terms that means the healthier and more active your multifidi muscles, the less likely you are to have low back pain!
Here is my favourite exercise for the multifidi. It is an extremely effective rehabilitation exercise and can even be performed by those with severe disc pain and can barely move. Re-educating the multifidi is also very important for those who experience recurrent episodes of their old disc problem. I have dubbed it ‘The Scarecrow’ as movement is minimal to avoid engaging the larger superficial back prime-mover muscles. Its focus is on stimulating and thereby restoring the sensory, inter-segmental stabilisation role of the multifidi as these muscles provide the important integrity, congruity and functional synchronicity between adjoining vertebrae.
The Scarecrow
Lie on your back with arms out at shoulder height, palms face up and feet hip-width, toes point up to the ceiling. Keep your eyes open and establish diaphragmatic breathing. Very slowly move your head and eyes to the right. At the same time move your feet slowly to the left. Coordinate the two so both your eyes and your toes come back to centre at the same time. Aim to get this action perfectly smooth, very slow and with your feet, eyes and head exactly coordinated. Jerky movements and/or an inability to co-ordinate feet and head is an indication of a lack of access to multifidus stimulation. Work up to 10 cycles, each one right and left.
An absence of leg pain carries a better prognosis, even when the leg pain resolves and back pain increases! In the absence of pain that extends down the leg spinal extension is often relieving and thereby recommended. The idea here is to move the disrupted nuclear material back towards the centre of the annulus. The degree of spinal extension should only be done to tolerance and may initially be as small and simple as lying on your belly, slowly progressing into a gentle Bhujangasana posture, Śalabasana, etc.
Also important is to avoid loading the spine in flexion, e.g.: sitting that causes a loss of the natural lumbar lordosis, forward bends if they are aggravating, poor postural habits of slumping, etc. Gentle movement like walking is a great activity to increase blood flow and helps with reabsorption of the disrupted disc material. After inflammation the body’s repair with collagen fibres can form adhesions along the nervous system. Post healing, flexion and extension of the spine causes the spinal cord and nerve roots to glide and is an excellent way to resolve adhesions.
HEALING
The annulus of the disc is a fibrous type of cartilage with no direct blood supply and is therefore very slow to heal. Without a set-back it usually takes around three months for natural healing to take its course. However, healing is often protracted and patchy with flare-ups and calmer periods so patience and persistence is needed. Factors that slow the healing process are the amount of static flexion loading, reinjury or previous episodes, smoking and diabetes. Discs repair themselves by filling the fissure with granulation tissue which means the disc become innervated at a deeper level so pain is felt sooner than in a healthy disc. Also, radial tears can reopen. As the granulation tissue is not the refined structure and as strong as the original intricate layers of collagen fibres, even once healed, the annulus is notoriously poor at regaining full tensile strength so extra caution needs to be taken to prevent future relapses.
If there is a failure to progress from rehabilitation and other conservative therapies, MRI is the imaging of choice. It can also screen for more concerning pathology as well as assess the dangers of neural compression. A radiograph or x-ray can only show how much disc height has been lost as it mostly captures the condition of the bony structures. CT scans, although much improved, still expose one to a very high dose of radiation. Surgery is not usually indicated for low back pain. It is a treatment for unretractable leg pain and/or progressive neurological deficit (e.g.: a loss of bowel/ bladder function, etc).
We may be born with predispositions to certain disease, however, understanding what enhances function and longevity of our joints and what prematurely destroys them gives us the opportunity to care for the temple we inhabit to the best of our abilities. In the case of discs, it is the nuclear matrix which determines the mechanical function of the spine. It has a vascular supply and draws fluid and nutrients from vessels in the vertebral bodies up to 1cm away! This osmotic pull plus movement is what drives this tide. If we lose the matrix we lose the drive of this vital tide. It is therefore important to recognize disc injuries in their early stage and treat them with the appropriate care to improve the chances of healing and prevent future recurrences.
With love and care
Monica
REFERENCES
Albert HB, Hauge E, Manniche C. Centralization in patients with sciatica: are pain responses to repeated movement and positioning associated with outcome or types of disc lesions?. Eur Spine J. 2012;21(4):630–636. doi:10.1007/s00586-011-2018-9.
Disc innervation image: https://basicmedicalkey.com/pain-of-spinal-origin-2/.
Feng Y, Egan B, Wang J. Genetic Factors in Intervertebral Disc Degeneration. Genes Dis. 2016;3(3):178–185. doi:10.1016/j.gendis.2016.04.005.
Kushchayev, S.V., Glushko, T., Jarraya, M. et al. ABCs of the degenerative spine.Insights Imaging 9, 253–274 (2018) doi:10.1007/s13244-017-0584-z.
Liebenson, Craig. Rehabilitation of the Spine: a Practitioner’s Manual. Lippincott, Williams and Wilkins. Baltimore, 1995.
Suri P, Hunter DJ, Jouve C, Hartigan C, Limke J, Pena E, Swaim B, Li L, Rainville J. Spine J. 2010 May;10(5):388-95. doi: 10.1016/j.spinee.2010.02.003.